Knee replacement is an operation that is performed principally to relieve pain from an arthritic knee. Although the range of motion of a knee may improve following surgery, this is not the primary aim of surgery and extra motion should be regarded as a bonus
SURGERY
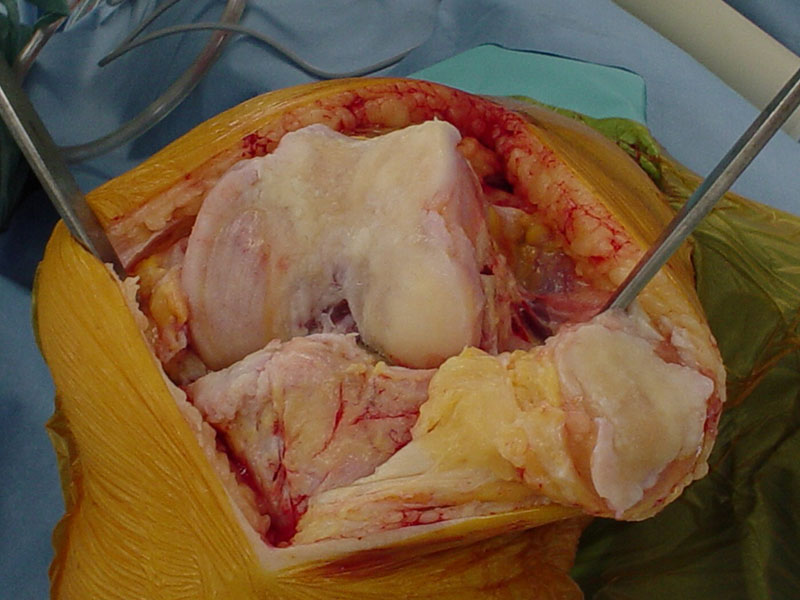
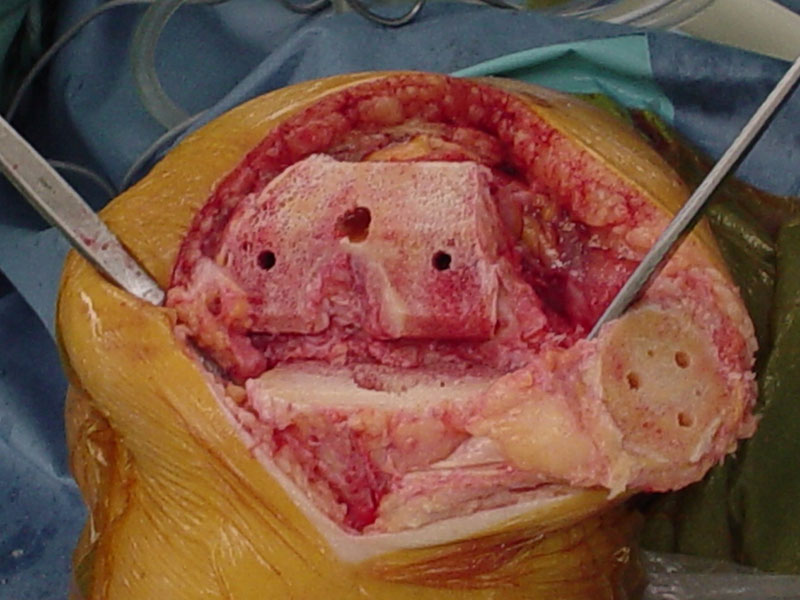
Knee replacement involves replacing the bearing surfaces on the ends of the bones with a synthetic surface. This is usually metallic on the femur and plastic (high-density polyethylene) with or without a metallic base plate on the tibia. The surface of the patella (knee cap) can also be replaced with high-density polyethylene.
Components can be fixed to the bone using one of two techniques. One can either use bone cement or one can use components coated in such a way that bone grows onto and into their surface. Both methods of fixation have their advantages and disadvantages. A decision will be made regarding the most appropriate fixation for your particular situation.
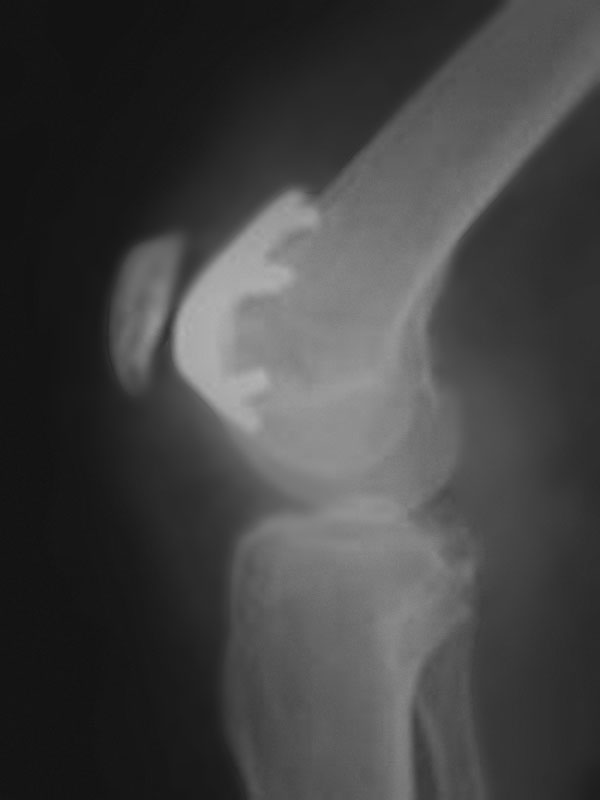
Depending on the nature of your arthritis, your knee may be suitable for a partial replacement rather than a total replacement. The knee can be thought of as having three compartments. There is a medial and a lateral compartment between the femur (thigh bone) and tibia (shin bone). The medial compartment is on the inside (left side of right knee) and the lateral compartment is on the outside (right side of right knee). The third compartment is between the patella (knee cap) and the femur.
In a total knee replacement, the medial and lateral compartments are replaced and the patella may be resurfaced as well. In a medial (or lateral) unicompartmental replacement only the medial (or lateral) compartment is replaced. Medial unicompartmental replacement is more common than lateral. Patellofemoral replacement involves resurfacing of only the patellofemoral compartment.
TOTAL KNEE REPLACEMENT

MEDICAL UNICOMPARTMENTAL REPLACEMENT

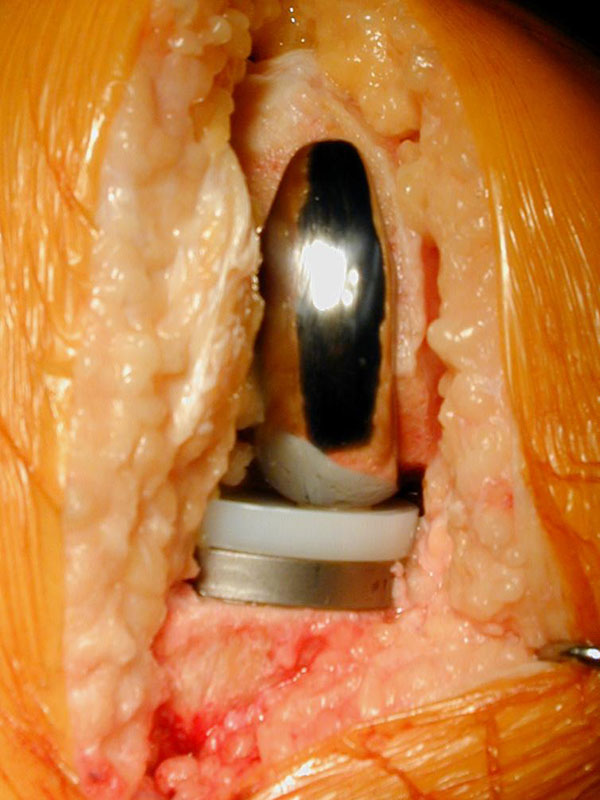

PATELLOFEMORAL REPLACEMENT

In general, the principles of partial and total knee replacement are similar but a partial replacement is a smaller operation and has a shorter hospital stay and quicker recovery.
As a rule of thumb, total knee replacement involves a hospital stay of 3-6 nights (2-5 for partial replacements). In most instances, patients are able to go directly home and inpatient rehabilitation is not usually required. Depending on your private health insurer, a physiotherapist may be able to visit you at home. When you are discharged you will be walking with the aid of walker support and will be independent in terms of showering and dressing.
The main problem that patients face after a knee replacement is getting their movement back. Pain levels vary considerably from one individual to another, but most people find the period from 24 hours to 72 hours after surgery the most difficult. It is important to keep working at the exercises, particularly bending the knee. This applies both in hospital and after discharge. Pain may persist for 6-8 weeks following the procedure, particularly at night.
PRE-ADMISSION
Prior to admission, a number of steps are taken to reduce the risks of surgery. A number of routine investigations may be performed and these include blood tests, an electrocardiograph (ECG), and analysis of a urine specimen. You may be asked to attend a pre-admission clinic at the hospital. The purpose of this clinic is to familiarise you with the planned surgery. If your knee X-ray is more than three months old a new X-ray may be taken, usually on admission to hospital.
You should preferably stop taking anti-inflammatory tablets one week before your surgery in order to reduce bleeding during the operation. You can take your normal painkillers as well as low dose (100mg) Aspirin if you are on this for cardiovascular reasons. If you are on anticoagulant medication such as warfarin or clopidogrel, it is important that you notify the doctors as soon as possible as you will need to cease these prior to surgery. Similarly, if you have an artificial heart valve or another implant that requires antibiotic protection when surgery is being performed, you should also notify the office staff.
ADMISSION
Admission to hospital is usually on the day of surgery. Occasionally you will be admitted earlier than this depending on your general health status.
ANAESTHESIA
The surgery can be performed using a number of different types of anaesthesia. The anaesthetist will select the most appropriate type of anaesthetic for your situation. Usually, a combination of spinal and general anaesthesia is used. A spinal anaesthetic involves an injection into the lower spine, which makes the body numb from the waist down. It wears off after a couple of hours.
AFTER SURGERY
Following surgery adequate provision is made for pain control. The anaesthetist and nursing staff will explain to you what is to be used in your situation prior to the operation.
Physiotherapy will commence on the first day following surgery. You will usually get out of bed on the afternoon of surgery if you have surgery in the morning, or the next morning if you have surgery in the afternoon. Initially you will walk with a walking frame and later with crutches. The physiotherapist will guide you through the various phases of rehabilitation. Depending on your surgeon’s preference, you may spend some time each day with your knee on a CPM (continuous passive motion) machine, which slowly bends and straightens your knee.
Usually, you can be discharged directly home from the hospital. The length of hospital admission varies considerably but is usually somewhere between 4-6 nights. You will not be discharged until you are safe to go home. This decision is usually made during your hospital admission. A follow-up appointment will be made for you, usually 2-4 weeks after the operation.
You will notice that your knee is warm and swollen for some time after surgery. This has usually settled significantly by three months from surgery, although the swelling may persist for a further few months. You will also notice that the skin on the lateral (outside) side of the incision will be numb. This is normal. The area of numbness usually decreases a little with time but there will always be some numbness of the skin in this area. However, it does not usually cause any problems.
RISKS
Knee replacement procedures are usually very successful. However, they are associated with some risks and although these are uncommon, they do need to be kept in mind in assessing whether this type of surgery is warranted. These risks include:
WEAR AND LOOSENING
With time, the bearing surfaces do have a tendency to wear. As a result, small particles of debris are produced. The body’s reaction to these particles can cause loosening of the components, which in turn can cause a recurrence of pain. This may necessitate a second (revision) operation, which is usually a significantly more complicated procedure and generally does not lead to as good a result as a primary procedure.
VENOUS THROMBOSIS
This is a blood clot in the veins of the leg and occurs more frequently after knee replacement surgery than other types of surgery. Precautions are taken to reduce the risk and this may involve the administration of a daily injection of a blood-thinning agent (low molecular weight heparin). Additional measures may be taken if it is felt that you are at greater risk than the average person undergoing surgery. If a venous thrombosis does occur this will usually need to be treated with blood thinning-injections followed by anticoagulant tablets (Warfarin), which would need to be continued for at least three months. A small but nonetheless important risk for venous thrombosis is the potential for the blood clot to break off and lodge in the lungs (pulmonary embolus). This can cause significant breathing problems and very rarely can be fatal.
INFECTION
Infection can occur after any operation. It is potentially more serious following joint replacement surgery, as it is more difficult to eradicate. This can mean that further surgery is required including the possibility of removal of both components for a period of two months during which antibiotics are given intravenously. If the infection has been eradicated, another knee replacement is then performed. Occasionally the knee may need to be permanently stiffened (arthrodesis). Precautions are taken to reduce the risk of infection including the administration of intravenous antibiotics around the time of surgery.
STIFFNESS
As mentioned earlier, the biggest challenge after a knee replacement is to regain knee movement, especially flexion (bending). Sometimes stiffness is a persistent problem and a manipulation under an anaesthetic is required. This involves coming back into the hospital, usually for one or two nights. Occasionally the stiffness may be permanent and may cause difficulties with activities of daily living.
Despite all of these potential problems, most patients are very happy with their procedure and recover quite quickly from surgery. However, it is important to remember that improvement occurs for up to 18 months after surgery.
Note: These notes have been prepared by orthopaedic surgeons. They are general overviews and information aimed for use by their specific patients and reflect their views, opinions and recommendations. This does not constitute medical advice. The contents are provided for information and education purposes only and not for the purpose of rendering medical advice. Please seek the advice of your specific surgeon or other health care providers with any questions regarding medical conditions and treatment.
